Understanding Venous Stasis Discoloration: Causes and Solutions

In the complex world of vascular medicine, one condition that often raises concern among patients and healthcare providers alike is venous stasis discoloration. This condition, characterized by changes in skin pigmentation due to poor blood circulation in the lower extremities, is not just a cosmetic issue; it signals underlying vascular health problems that require attention. This article will explore the various facets of venous stasis discoloration, detailing its causes, symptoms, and available treatments, with insights from leading professionals in the field, particularly those from Truffles Vein Specialists.
What is Venous Stasis Discoloration?
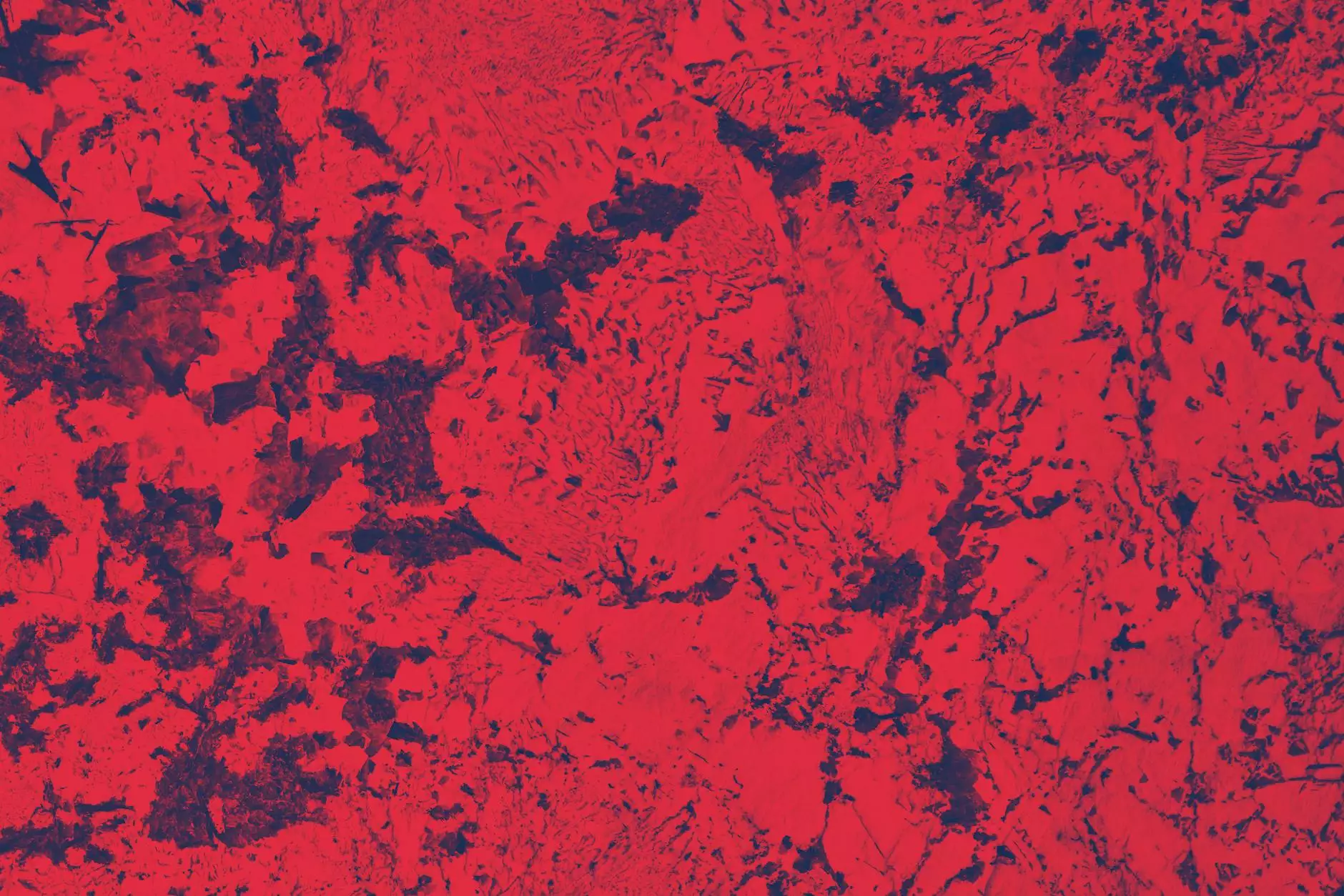
Venous stasis discoloration refers to dark, often reddish-brown patches that typically appear on the skin of the lower legs. These changes in skin color are a direct result of chronic venous insufficiency (CVI), where the veins fail to adequately return blood from the legs back to the heart. This inadequate circulation often leads to the accumulation of blood and fluid, causing pigmentation changes.
Causes of Venous Stasis Discoloration
Several factors contribute to the development of venous stasis discoloration. Understanding these causes can aid in prevention and management. Here are some of the primary contributors:
- Chronic Venous Insufficiency (CVI): The most significant cause, where vein valves do not function properly.
- Age: Older adults are more susceptible due to weakened vein walls and valves.
- Obesity: Excess weight increases pressure on the veins, leading to complications.
- Pregnancy: Hormonal changes and increased blood volume can lead to venous issues.
- Prolonged Sitting or Standing: Occupations that require long hours in one position can exacerbate poor circulation.
- Previous Venous Thrombosis: A history of blood clots can damage veins and lead to CVI.
Symptoms Associated with Venous Stasis Discoloration
Identifying the symptoms of venous stasis discoloration is crucial for early intervention. Key symptoms may include:
- Skin discoloration: Visible dark spots or patches on the lower legs.
- Swelling: Increased swelling in the lower legs and ankles.
- Skin changes: Skin may become thickened or leathery.
- Itching or discomfort: Some patients report itching or a feeling of heaviness in the legs.
- Ulcers: In severe cases, ulcers may develop due to long-standing stasis.
The Impact of Venous Stasis Discoloration on Quality of Life
The presence of venous stasis discoloration can significantly impact an individual's quality of life. Not only can it affect physical health, but it can also lead to emotional distress. Many individuals feel self-conscious about their appearance, which can limit social interactions and impact mental well-being. Furthermore, the discomfort can make daily activities challenging.
Diagnosis of Venous Stasis Discoloration
Diagnosing venous stasis discoloration typically involves a comprehensive evaluation by a vascular specialist. The diagnosis process may include:
- Medical History Review: Discussing symptoms, lifestyle factors, and family history.
- Physical Examination: Inspecting the legs for discoloration and other symptoms.
- Doppler Ultrasound: This non-invasive test assesses blood flow in the veins and identifies any blockages or reflux.
- Blood Tests: Used to rule out other causes or complications such as thrombosis.
Treatment Options for Venous Stasis Discoloration
Treating venous stasis discoloration involves addressing the underlying causes and managing symptoms. Treatment options may include:
Conservative Measures
For mild cases, conservative treatments are often effective. These may include:
- Compression Therapy: Wearing compression stockings can help improve blood flow and reduce swelling.
- Elevation: Regularly elevating the legs can aid circulation, especially after long periods of sitting or standing.
- Weight Management: Maintaining a healthy weight reduces pressure on the veins.
- Exercise: Regular physical activity helps to strengthen veins and improve circulation.
Medical Interventions
When conservative measures are insufficient, medical interventions may be needed:
- Endovenous Laser Therapy (EVLT): A minimally invasive procedure that uses laser to close off varicose veins.
- Radiofrequency Ablation: This technique uses heat to treat varicose veins.
- Sclerotherapy: Involves injecting a solution into the affected veins to collapse and fade them.
Preventing Venous Stasis Discoloration
Prevention is always better than cure. Here are some effective strategies to reduce the risk of developing venous stasis discoloration:
- Stay Active: Regular physical activity enhances blood circulation.
- Avoid Prolonged Sitting or Standing: Take breaks and move around to promote circulation.
- Use Compression Garments: Especially during long flights or sitting periods.
- Stay Hydrated: Proper hydration can support vascular health.
- Manage Underlying Conditions: Controlling diabetes, hypertension, and other health issues is crucial.
Conclusion
Venous stasis discoloration is more than just a cosmetic concern; it is a sign of deeper health issues that deserve attention. By understanding the causes, recognizing symptoms, and exploring treatment options, individuals can take proactive steps toward managing this condition. Experts at Truffles Vein Specialists are dedicated to providing comprehensive care, helping patients regain not just their skin’s appearance but their overall health and well-being. If you suspect you are experiencing venous stasis discoloration, don’t hesitate to consult a healthcare professional for an accurate diagnosis and effective treatment plan.